Abstract
Background
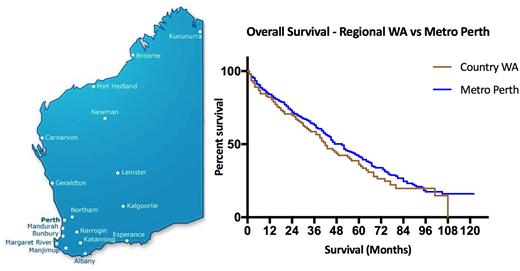
There has been concern that patients with malignant disease from remote and regional country areas may have adverse outcomes compared with those from cities. Western Australia (WA) with an area of 2,526,786 square kilometers, is one third the size of Australia. It has a population of 2.6 million of which 92% live in the capital city Perth and the southwest corner. In WA, multiple myeloma is managed in tertiary public hospitals and private physician practice located in Perth. While oral based immunomodulators and alkylators are readily delivered in the regional areas, patients travel to Perth for parenteral chemotherapy and stem cell transplantation. The WA state government subsidizes transport and accommodation for patients from regional areas to travel to Perth for treatment and clinical review via the Patient Assisted Travel Scheme (PATS). Telehealth through video conferencing is also used for review of patients on oral-based anti-myeloma treatment or during surveillance periods to avoid expensive and time-consuming travel to Perth. The Royal Flying Doctor Service (RFDS), a non-profit medical organization, provides prompt transfer of unwell patients from regional and remote areas of WA to Perth. Pathology services in remote regions are provided by the publicly funded PathWest organization.
Method
We retrospectively reviewed the survival outcomes of patients with multiple myeloma in the WA public healthcare system. Patients diagnosed between 2008 to 2017 were included (n=569). Staging information was extracted from the laboratory information system and the cytogenetic database in PathWest. Patient demographics, complications requiring admission, mortality and follow-up data were extracted from the public hospital patient management systems. Patients were segregated into regional or metropolitan by their residential address postcodes. Patients diagnosed and/or followed-up in the private sector were excluded. Survival was analyzed by Kaplan-Meier curves, Log-rank test and Cox proportional hazards model.
Result
Median age at diagnosis was 67 years old (range 29 to 98), with 56% above 65 years. 56% were males, 44% were females. Overall median survival was 46 months (95%CI:41,52). 1-year, 3-years and 5-years survival rates were 80%, 56% and 30% respectively. 25% (n=143) of patients resided in regional areas. No statistically significant difference in overall survival time between patients from metropolitan and regional areas was identified (p=0.2): 47 months (95% CI:43,54) and 42 months (95% CI: 33,54) respectively. Subgroup analysis also did not find any significant difference in overall survival of each R-ISS staging between metropolitan and regional areas.
Discussion
This retrospective study provides real-life survival data of of an Australian-based population in a state with a large land mass and low population density outside the capital city. The overall survival of patients living in regional areas was not significantly different from those living in the capital city. This gives credence to the benefit of the WA government supported regional network of travel, accommodation and Telehealth conferencing overcoming the distance barrier in the provision of comprehensive medical care in the management of a hematological malignancy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal